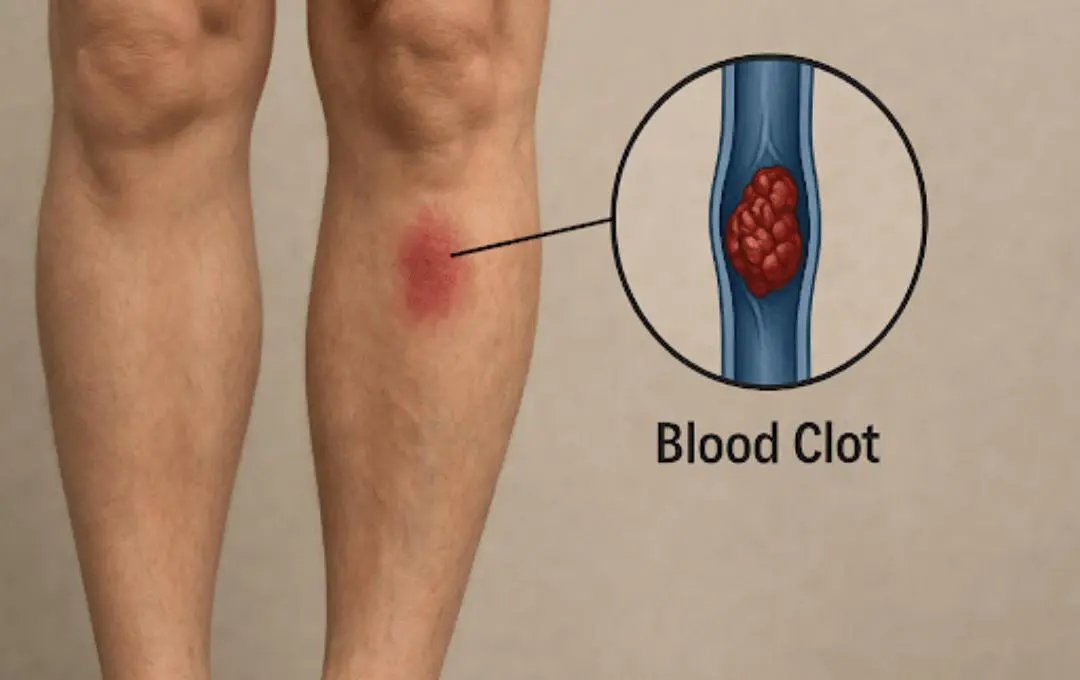
Blood clots are not only a serious health concern but can also happen without warning. Deep vein thrombosis (DVT) is the most common type of blood clot, and can become life-threatening if it travels to the lungs and causes a pulmonary embolism (PE). However, many blood clots are preventable, so understanding the causes of DVT and PE can help support healthy circulation.
Varicose veins can increase the risk of DVT, so let’s explore how varicose veins and other risk factors increase the risk. Additionally, this blog will discuss the symptoms of DVT and PE, as well as how one can prevent them from occurring. It may involve a potential vein treatment to limit the risk.
What Increases Your Risk of Blood Clots?
Blood clots typically develop when blood flow becomes abnormally thick or slows due to an injury to a blood vessel. In the case of varicose veins, the damaged vein valves that cause the bulging appearance may mimic the body’s response to an injury. Because varicose veins can be a chronic condition, the blood clot may not dissolve, which can further impede blood flow.
Common risk factors of blood clot formation include:
- Long periods of inactivity (travel, recovery after surgery, or a sedentary lifestyle)
- Vein disease or chronic venous insufficiency (CVI)
- Heart conditions (heart failure and atrial fibrillation)
- Pregnancy or hormone replacement therapy
- Obesity
- Smoking
- Family history of clotting disorders
How Blood Clots Progress: From DVT to PE
DVT typically forms in a deep vein in the legs. A pulmonary embolism forms when a blood clot breaks off and travels to the lung, restricting blood flow. This is dangerous because it affects your body’s oxygen levels and can damage other organs.
DVT and PE may not cause a specific sensation, but they can produce symptoms indicating that you need medical attention.
Symptoms of Deep Vein Thrombosis (DVT):
- Persistent swelling in the calf or leg, usually on one side
- Tenderness or pain in the calf or thigh, especially when walking or exercising
- Redness or warmth in the affected area
- Discomfort or tightness in the calf
Pulmonary Embolism (PE) Symptoms:
- Sudden shortness of breath
- Sharp or stabbing chest pain that worsens while taking deep breaths
- Dizziness
- Coughing up blood
Many vein conditions develop gradually without obvious symptoms at first. However, neglecting treatment can increase the risk of developing conditions such as DVT and PE. Scheduling a consultation with a vein doctor can help identify circulation issues or vein disease before clots even form.
MEET WITH AN EXPERIENCED VEIN DOCTOR
How To Avoid Deep Vein Thrombosis
Deep vein thrombosis prevention is critical to reducing the risk of pulmonary embolism. Certain DVT risk factors can be managed with lifestyle changes and proper vein treatment.
Regular Exercise and Movement
A sedentary lifestyle can slow blood circulation and increase the risk of DVT. Incorporate simple movements into your day to prevent deep vein thrombosis. Here are a few ways to stay active and support healthy circulation throughout the day:
- Consider adding a stretching or yoga routine.
- During long car rides, stop every two to three hours to walk around or stretch.
- If you sit for extended periods, try to get up every hour.
Manage Risk Factors That Increase Clotting
Controlling risk factors like weight, diet, and chronic conditions like high blood pressure and cholesterol helps prevent blood clots. This type of control includes exercising for at least 150 minutes a week, as recommended by the National Institute on Aging. Additionally, eating a balanced diet of fresh fruits, vegetables, and lean proteins such as salmon, tuna, eggs, and low-fat dairy supports vein health. Limiting smoking and alcohol consumption is also recommended.
Know Your Family History
Having close relatives who have experienced clotting disorders, deep vein thrombosis, or pulmonary embolism increases your risk of DVT. It’s important to share this information with your healthcare provider so they can run the necessary screenings and recommend preventive measures.
Pulmonary Embolism Prevention

Tips to Reduce The Risk of Blood Clots in the Legs
Supporting healthy blood circulation can help prevent blood clots from forming. Here are a few effective ways to naturally reduce your risk:
Wear Compression Stockings
Compression stockings can help lower the risk of blood clots, especially if you stand or sit for long periods, have recently had surgery, or travel frequently. These stockings apply gentle, graduated pressure to the lower legs to improve circulation and prevent blood from pooling.
Elevate Your Legs at the End of the Day
Elevating your feet while relaxing or sleeping can improve circulation and help relieve common vein disease symptoms such as swelling, aching, and discomfort.
To elevate your legs effectively, use pillows to raise them to a level above your heart. This helps blood return to the heart more efficiently and reduces pressure in your leg veins.
Stay Hydrated
Proper hydration helps prevent blood clots by supporting healthy blood flow. When your body is dehydrated, your blood can become thicker and circulate more slowly, increasing the risk of clot formation. Drinking plenty of water, as well as fluids like fresh fruit juice, tea, or vegetable juice—helps keep your blood moving smoothly and reduces your risk.
Vein Treatments for Long-Term Blood Clot Prevention

A timely diagnosis and treatment reduce the risk of future blood clots, prevent chronic swelling, skin changes, or post-thrombotic syndrome, and improve circulation while enhancing mobility.
Our vein doctors use advanced, non-invasive diagnostic tools, such as venous ultrasound, to detect circulation problems before they become severe.
This treatment plan may include one out of several minimally invasive treatments to improve circulation and help prevent blood clots from forming, including:
- ClariVein®
- VenaSeal™
- Varithena
- Radiofrequency Ablation
- Ultrasound-Guided Sclerotherapy
- Endovenous Laser Vein Treatment
- Sclerotherapy
These non-surgical treatments seal or close off damaged veins, restoring proper blood flow, reducing the risk of clot formation, and preventing further complications.
If you are experiencing symptoms of vein disease like leg pain, swelling, or visible veins, USA Vein Clinics can help. We accept most insurance plans, including Medicare and Medicaid. You can schedule an appointment online to instantly verify your coverage.
Frequently Asked Questions
What Does a Pulmonary Embolism (PE) Feel Like?
Pulmonary embolism (PE) can present with a range of symptoms, often beginning with sudden, sharp chest pain that worsens with deep breaths or coughing. Shortness of breath can develop quickly, varying from mild to severe, along with dizziness, lightheadedness, or even fainting. You may still feel symptoms of deep vein thrombosis (DVT), such as leg pain, swelling, or redness in one leg.
How Long Does it Take for a DVT to Become a Pulmonary Embolism?
The highest risk of DVT becoming a pulmonary embolism occurs within the first few days to four weeks after the clot forms. How quickly a clot travels to the lungs depends on its size, location, and an individual’s overall health.
Can a Blood Clot Go Away On Its Own Without Treatment?
Smaller blood clots can dissolve naturally on their own. However, larger clots or those located in critical areas, such as the lungs or brain (stroke), require prompt medical treatment to avoid serious complications.
Can You Have a Blood Clot with No Symptoms?
It’s possible to have a blood clot without noticeable symptoms. It is estimated that about half of those affected by DVT experience no symptoms at all or only mild ones that are easy to overlook. A pulmonary embolism (PE) can also happen without any prior symptoms of deep vein thrombosis (DVT).
Symptoms can include swelling, pain, or warmth in a limb, which may indicate deep vein thrombosis (DVT). For pulmonary embolism (PE), symptoms can include chest pain or shortness of breath. Always seek medical attention if you notice any of these warning signs.
Medically Reviewed By:
Dr. Yan Katsnelson is a philanthropist, business owner, and highly skilled cardiac surgeon. He is the Founder and CEO of USA Vein Clinics, which is part of USA Clinics Group, the parent company of USA Fibroid Centers, USA Vascular Centers, and USA Oncology Centers, with more than 100 facilities nationwide. Dr. Yan has established himself as a strong advocate for accessibility and affordability of the most advanced medical care close to home. His mission is to create a positive experience for each patient with compassionate, personalized, and expert care.